Understanding Addiction & Borderline
Personality Disorder
Borderline personality disorder (BPD) is a mental illness characterized by emotional instability, poor interpersonal relationships, suicidal ideation and attempts, sensitivity to rejection, and fear of abandonment. Early research suggested that, as a disorder, BPD was resistant to medical treatment, leaving those with the disease lost and confused. Though there are treatments available today, diagnosing the issue accurately has been a challenge.

Unfortunately, our culture has been quick to label and dismiss people who suffer from most mental illnesses, but it is particularly true with BPD because of the type of behavior these people exhibit. Stereotypes of BPD sufferers include being high maintenance, attention seeking, overly sensitive, or a combination of these. Any of these symptoms, taken alone, is easily dismissible.
Because people often dismiss these people without treatment, diagnosis, or care, many self-medicate through alcohol, prescription drugs, or illicit drugs. Once this starts, it can quickly lead to addiction and a cycle of substance abuse.
What Is BPD?
BPD is one of several personality disorders that are often diagnosed with substance abuse. It is a multifaceted and serious mental illness, and the opportunity for misdiagnosis is high. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5), defines a personality disorder by describing six diagnostic criteria:

- Imbedded patterns of behavior that stray significantly from the typical expectations of behavior of the person’s culture.
- Behavior patterns that are inescapable, obstinate, and expected to change.
- Appearance of the disorder’s symptoms no later than early adulthood (unlike depression, which doesn’t discriminate against age).
- Absence of cognizance that behavior patterns and personality features are problematic or that they fluctuate from those of other persons.
- Grief and impairment in one or more parts of an individual’s life (frequently only once other individuals get distressed about his or her conduct).
- Substance abuse, medication, or some other mental disorder or medical condition (such as a head injury) are not the causes of behavioral patterns, though they can exacerbate the condition.
Causes And Risks Of BPD
The development of our personalities is a mystery. We do know some things, however. Behavior, environment, and cognition shape our personalities. Researchers believe that BPD originates in childhood but doesn’t manifest until adulthood. As a child, the sufferer may face traumatic experiences, like abuse, which fuel the mental illness, but the disorder doesn’t surface until early adulthood. Though abuse seems to be a factor, the exact cause of BPD is unknown.

A dysfunctional family environment places an individual at an increased risk of developing BPD. While not all BPD sufferers have traumatic childhoods, the majority of them do. Physical, emotional, and sexual abuse are linked to an increased risk of an adult BPD diagnosis, as is abandonment. BPD symptoms serve as coping mechanisms for the emotional trauma of a difficult upbringing.
Genetics and neurology, however, may also be factors. If a close relative, such as a parent, has the disorder, then subsequent offspring are predisposed to developing it. Additionally, if brain areas that house mood, behavioral, and emotional center suffer abnormalities, they can result in BPD, with symptoms ranging from unpredictable mood, impulsive behavior, and unstable emotions.
The mystery of nature versus nurture also comes into play. Do people develop BPD because of the cycle of childhood abuse, or is in their DNA? Currently, there isn’t enough research for definitive answer.
How BPD Sufferers Become Addicts
Though they’ve often sought treatment, medical professionals have often misunderstood those with; some assume it isn’t treatable and others misdiagnose it completely. Adding to this is often a reluctance to be open with or trust mental health professionals, whom they may see as untrustworthy or as targets for manipulation. Because the effects of the illness can be so disabling and because few options seem available, many people suffering with BPD turn to drugs and alcohol to dull symptoms.
Compounding the challenge of treating BPD is addiction. Nearly half of those who suffer from BPD are addicts as well. It is important that an individual with a dual diagnosis, which is the parallel existence of two mental health disorders, receive an individualized treatment plan. Alcohol, cannabis, cocaine, heroin, and prescription medications are among the substances sufferers use to ease symptoms of BPD, though these chemicals often exacerbate the underlying issues.
Why BPD Sufferers Are At Higher Risk For
Substance Abuse
 BPH patients experience fear of abandonment, paranoid thoughts, and a range of unstable emotional pain. These symptoms lead to altered self-awareness and disturbed interpersonal relationships. Desperate for relief from these afflictions, those with BPD look to drugs and alcohol. Unfortunately, these attempts generally backfire. Substance abuse intensifies BPD’s symptoms like depression and rage, and it increases the risk of self-harming behaviors and suicide attempts.
BPH patients experience fear of abandonment, paranoid thoughts, and a range of unstable emotional pain. These symptoms lead to altered self-awareness and disturbed interpersonal relationships. Desperate for relief from these afflictions, those with BPD look to drugs and alcohol. Unfortunately, these attempts generally backfire. Substance abuse intensifies BPD’s symptoms like depression and rage, and it increases the risk of self-harming behaviors and suicide attempts.
Rigorous, client-specific treatment can yield a positive prognosis, absent of relapse, according to an evidence-based BPD article from September/October 2016 in the Harvard Review of Psychiatry. Successful treatment can come, however, from understanding how BPD fuels addiction.
How Borderline Personality Disorder
Was Discovered
Several decades ago, physicians thought BPD was a branch of schizophrenia. Treatment depended on how a person’s schizophrenia (or what was actually BPD) manifested. If a client had neuroses, they were considered examinable, and, therefore, fixable. If a client possessed psychoses, on the other hand, doctors considered the examination impossible, and, therefore, not fixable.
Because they misdiagnosed BPD as schizophrenia, patients were improperly – and sometimes dangerously – treated. In the late 1960s, however, physicians began to see BSD as a separate disorder but still connected to schizophrenia. They categorized it as both neuroses and psychoses. For doctors during this time, issues that marked the illness were desperate needs for attention, serious attachment to others, and fear of abandonment.
In the 1970s, doctors labeled BPD as another syndrome and called it borderline personality disorder. In fact, BPD has starkly opposite characteristics from schizophrenia, which evidences decreased emotions and decreased personal attachment. BPD sufferers have increased emotions and increased personal attachment. During this decade, treatment for the newly minted illness focused on psychoanalytic therapy.
How BPD Becomes Distinctive From Other Disorders
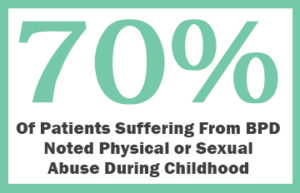 During the 1980s, BPD received much more attention than it had before, and, eventually, researchers realized BPD was a separate disorder from depressive disorder, because neither of these two showed medication commonalities. It was also during this time that researchers made a connection between BPD and childhood abuse. They noted physical or sexual abuse during childhood in 70% of BPD clients. Treatment modalities centered on extending empathy and support to the BPD sufferers. Though there is less hard research, childhood abandonment also seems to be a factor.
During the 1980s, BPD received much more attention than it had before, and, eventually, researchers realized BPD was a separate disorder from depressive disorder, because neither of these two showed medication commonalities. It was also during this time that researchers made a connection between BPD and childhood abuse. They noted physical or sexual abuse during childhood in 70% of BPD clients. Treatment modalities centered on extending empathy and support to the BPD sufferers. Though there is less hard research, childhood abandonment also seems to be a factor.
In the 1990s, however, the validity of how physicians diagnosed the disease was challenged. Some thought that if certain medications could successfully erase the disorder, then diagnosis meant it could be treated and eradicated. Also during the 1990s, dialectical behavior therapy and mentalization-based treatments were developed and often used to treat BPD.
Developments That Expanded BPD Treatment
From 2000 to 2009, researchers discovered that BPD was more likely to occur in individuals whose immediate family – first generation – also had BPD. Enhanced treatments benefited the client and family. From psychoeducation to specialized medication, treatment showed promise, and those with BPD had hope. Awareness of the illness spread, and, in 2005, May became Borderline Personality Awareness Month in the United States.
Though awareness is crucial, BPD remains an issue. Because of public awareness, extensive research studies led to greater empathy for those with the disorder, a better treatment, and a deeper understanding of the theories that define BPD.
The Prevalence Of BPD
In the United States, BPD affects 1.6% to 5.9% of the population, though these are only the cases that have been diagnosed. Many addicts suffer from mental illness and addiction but receive treatment only for the addiction. Of those being treated for mental health issues, 10% of mental health outpatients will have BPD, and 20% of mental health inpatients have BPD.
Of those being treated for mental health issues, 10% of mental health outpatients will have BPD, and 20% of mental health inpatients have BPD.
A person’s gender may affect the specific symptoms of BPD. It’s three times more prevalent in females than males. The most common dual diagnosis disorders in women with BPD are anxiety, eating disorders, major depression, and post-traumatic stress disorder (PTSD). The key dual diagnosis disorders seen in men with BPD are antisocial personality disorder, explosive anger episodes, and substance abuse disorder.
Onset Of BPD And Symptoms
BPD generally shows itself in early adulthood, with symptoms varying depending on factors such as gender, childhood abuse, genetics, and neurology. Though some adults have specific incidents that trigger the illness, there is no one particular trigger; it seems to be induced by normal events.
Some symptoms of BPD are also characteristic of other psychiatric disorders. Because of this, a mental health professional who has a history of diagnosing disorders should assess a potential BPD client over time for an accurate diagnosis. However, a few symptoms distinctive to BPD are:
- Sensitivity to Criticism
- Sensitivity to Rejection
- Fear of Abandonment
Other symptoms of BPD are more general, and, as such, are easily confused with other mental illnesses. A few of these can include:
- Actions of self-harm or suicidal attempts. Self-mutilation through cutting and patterned suicidal behavior are evidenced. These include cutting, skin picking, skin burning, hitting, and hair pulling. Sexual abuse can play a role in increasing suicidal attempts in teens with BPD.
- A coping mechanism used to escape certain situations, leave an environment, or detach oneself from an experience. If a BPD client experiences stress in a certain location, for example, a hospital, that person will make all sorts of attempts to avoid going there. If a BPD client experienced a traumatic event in childhood, the patient may make efforts to avoid talking about it. Dissociation can range from mild to severe.
- Fear of abandonment and desperate efforts to avoid real or perceived desertion. BPD clients may fear the ending or failure of a relationship, regardless if it’s a reasonable possibility. BPD clients may go to extreme effort to avoid ending a relationship due to a fear of abandonment.
There are many other symptoms, but taken alone, they can be easily dismissed or be too vague for a clear diagnosis. Symptoms can include feelings of emptiness, impulsive behavior, paranoia, and unstable relationships. Black-and-white thinking may also be a symptom. On their own, however, these symptoms may not offer physicians and mental health experts enough to diagnose BPD decisively. Discovering whether someone has BPD is crucial. In extreme cases of the illness, sufferers can break from reality and have psychotic episodes.
BPD’s Distinctive Sign: Suicide Attempts
BPD is the only mental disorder that includes attempted suicide or self-harming behaviors in its diagnostic criteria. BPD clients have a 50 times higher suicide rate than the rest of the U.S. population, and nearly 8 in 10 BPD clients report attempting suicide.

Likewise, non-suicidal self-injury (NSSI) is common among people with BPD, with a prevalence of greater than 75%. Cutting is one example of an NSSI, whereas a suicide attempt indicates a desire to die, an NSSI does not. Individuals with BPD report various reasons for committing an NSSI, ranging from an anger expression outlet to an attention grabbing display.
Treatments For BPD
Because addiction often masks BPD symptoms, diagnosing this particular mental illness can be challenging. Once diagnosed, treatment can be difficult, for both the sufferer and the person trying to help. Health care professionals often bear the brunt of emotional outbursts and attention-seeking behaviors.
There have been certain treatments that physicians have seen successfully help people with BPD. A few are:
- Cognitive Behavioral Therapy (CBT)
- Electroconvulsive Therapy (ECT)
- Metallization-Based Treatment
- BASE Cognitive-Affective Treatment Approach
- Symptomatic Medication Treatment
- Mental Health Hospitalization
Like with many mental illnesses, there are no cures for BPD, but specialized treatments – some of which can combat addiction as well – offer hope to those who are afflicted with this disease.
BPD treatment responses vary depending on the individual. Due in part to dissatisfaction and depression, 10% of BPD clients die from suicide. However, long-term BPD prognoses are positive, with 50% showing an improved condition in 10 years.
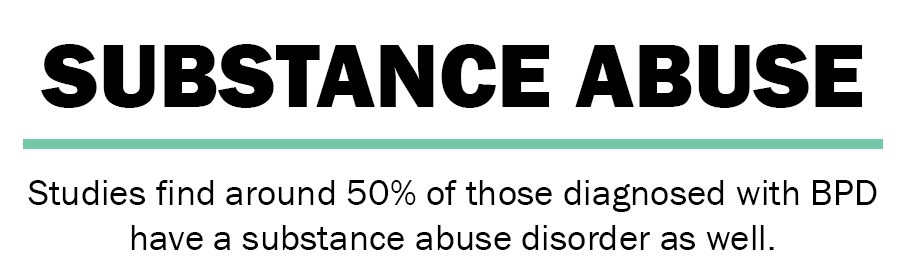
The Complex Relationship Between BPD And Substance Abuse
As we’ve seen, people with BPD often combat the disease through substance abuse. There have been several worldwide studies conducted to explain the correlation between BPD and drug use. Studies find around 50% of those diagnosed with BPD have a substance abuse disorder as well. Though many are self-medicating, one Brazilian study suggested that the high-risk and self-harm components of the disease increase drug abuse in those with it. The most commonly abused substances were alcohol, cannabis, and cocaine.
Drug use heightens symptoms of BPD, although they are severe enough on their own. Drugs and alcohol intensify impulsive behavior and increase suicidal tendencies. One longitudinal study showed that 62% of BPD individuals were addicts at the start of the study.
There are several symptoms that BPD and addiction share, making an accurate diagnosis of either disorder difficult. Both BPD and addiction exhibit:
- Decreased Self-Concern
- Depression
- Impulsive Behavior
- Increased Risk-Taking Behavior
- Manipulation
- Paranoia
- Range of Moods
- Self-Destructive Behavior
- Unstable Relationships
To give clients who have both BPD and substance abuse successful treatment, clients must have their substance abuse (their comorbidity) disorder correctly diagnosed and their personality characteristics noted. Though they share many symptoms, understanding whether BPD is part of a person’s addiction is vital to his or her therapy.
BPD And Substance Abuse
Dual Diagnosis Challenges
A dual diagnosis of BPD and substance abuse presents with several treatment challenges, the first of which is determining that both diseases are at play and perhaps fueling each other. Personality disorders are persistent, and those with BPD often oppose their health care professional’s orders and do not follow treatment advice – an unfortunate aspect of the disease.
BPD sufferers, perhaps at least in part due to prior traumatic life events, struggle with significant feelings of anger when a trigger arises during therapy. Therefore, those with the illness, therapists, and additional health care team members involved in the person’s care must be diligent about establishing a healthy relationship among each another. Similar to their patterns of instable relationships, individuals with BPD may shift from one therapist to another, never establishing long-term history and continuity of care, due to a false perception that each therapist is not the therapist for them.
Between the defiance the illness causes, as well as the instability of relationships, BPD sufferers can be their own worst enemies, for both treating their mental illness and their addiction.
Dual Diagnosis Treatment Plans For BPD Sufferers With Substance Abuse Issues
Dual diagnosis clients who receive care for BPD with one professional while pursuing substance abuse care with a different professional must ensure both professionals collaborate in their treatment or else all aspects of treatment will be complicated. Generally, professionals find that using a team approach to treating a dual diagnosis client is most effective. For example, a client may have a therapist, a group therapist, a psychiatrist, and others. Again, it’s imperative that these health care providers meet regularly to discuss treatment options and progression for each person they treat.
Keep in mind that BPD clients manifest manipulative behavior. Therefore, they may try to ruin the treatment plan by giving contradictory information to each provider or by attempting to turn the team against one another. Because of this, team members must be diligent in their communication, and plan for such behavior.
When people have a BPD diagnosis, providers should monitor them for symptoms of substance abuse. They may be reluctant to admit to drug abuse and addiction for many reasons – the most crucial of which may be fear of the drugs being unavailable. Understanding and explaining the relationship to those with these diagnoses is crucial to their recovery. Some approaches to treatment for dual diagnosis for BPD and substance abuse are:
Mentalization-Based Treatment
Mentalization-based treatment addresses the theory of many who study BPD that clients have a challenging time forming a mental picture of their self-awareness or emotions, feelings, or beliefs. A study has revealed a successful decrease in suicide attempts with this type of treatment.
BASE Cognitive-Affective Treatment
BASE therapy helps people with BPD alter conscious thinking and behaviors. The focus is on decreasing or eradicating lethal symptoms of the illness and improving quality of life. BASE treatment attempts to reverse negative thinking and instill trust, hope, and adaptive thinking. The program doesn’t only convey this information to client; it promotes a family environment within group sessions. Reviews of the program are positive, with clients expressed a sense of belonging, being included, and not looked down upon.
Schema Therapy
Dr. Jeffry Long rightly understood that ignoring a child who expresses a desire to see Dad or Mom leads to devastating adult symptoms. 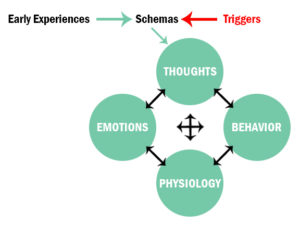 Instead of punishing children by leaving them alone in a room to think about what they did or neglecting to show interest when a child cries, a parent should nurture, comfort, and console to instill positive foundations of coping, attachment, safety, acceptance, and love. This theory blends multiple theories together, including cognitive behavioral therapy (CBT).
Instead of punishing children by leaving them alone in a room to think about what they did or neglecting to show interest when a child cries, a parent should nurture, comfort, and console to instill positive foundations of coping, attachment, safety, acceptance, and love. This theory blends multiple theories together, including cognitive behavioral therapy (CBT).
The goals are four-fold – assist the client to stop using maladaptive behavior, reconcile prior manipulative schemas, shut down maladaptive schemas from the past, and use daily life events to satisfy emotional needs.
Pharmacologic Therapy
Currently, the Food and Drug Administration (FDA) has not approved pharmacologic medication for BPD treatment specifically.
Nevertheless, there are medications available to manage the disorder symptomatically. Selective serotonin reuptake inhibitor (SSRI) anti-depressants (as mentioned previously for BPD treatment) are not only taken to treat depression but are also used to target irritability, impulsivity, and anger.
The FDA has approved medications for the treatment of substance abuse. Medications to treat alcohol abuse include:
- Acamprosate
- Disulfiram
- Naltrexone
Medications to treat opioid abuse, ease the pain of withdrawal, and decrease cravings include:
- Buprenorphine
- Methadone
- Naltrexone
Of course, medication should be only one portion of the treatment plan. Other treatment modalities include individual therapy, group therapy, and mutual-help groups. Though these medications don’t treat BPD specifically, they do help those with a dual diagnosis feel as if they are on the path to recovery once they feel some release from addiction.
Relapse Prevention Training For Dual Diagnosis BPD/Substance Abuse Clients
Increased relapse rates for a dual diagnosis client necessitate relapse prevention training. This involves group therapy, which works to encourage discussion about multiple clients’ challenges, successes, and effectiveness of each other’s’ coping mechanisms.
Though not specifically for BPD, those with the illness have found SSRI antidepressants to be effective in managing some symptoms. These drugs help to replenish the brain’s level of neurotransmitters.
How To Work With A Dual Diagnosis BPD/Substance Abuse Client
Health care professionals in various specialties of mental health, families, and friends will be better equipped to help a dual diagnosis BPD/substance abuse client by knowing the cause and effects of both disorders. Working with knowledge of only one when someone suffers both can seriously hamper recovery.
When health care providers are working with a dual diagnosis client, there are a few important factors to keep in mind. A professional should:
- Be aware of the impulsiveness of BPD. A client may cause harm to self or attempt suicide.
- Understand that communication among the treatment team members is important in meeting the needs of someone with BPD. Facilitating those meetings is crucial.
- Dedication to self-care. Mental health care professionals should schedule BPD clients before lunch or another break because their needs can be extensive, as can their dependence on the health care provider. Also, it’s important not to schedule BPD clients one after another.
- Firm professional boundaries. Health care professionals – especially therapists – should establish clear boundaries with the BPD patients they treat from day one. Tell them how long appointments will be, the proper method of contact, and how much support to expect. Boundaries should be firmly reinforced but not with rigidity. Be hesitant to make exception to the initially established rules, because the manipulative nature of someone with BPD may try and further push boundaries. Clients may attempt to gain a further level, or greater number, of exceptions over time.
- Understand that working with someone with BPD has unique challenges; be prepared for them.
Whether you are suffering and looking for help or you are trying to help someone you love, understanding treatment protocols and options can make the transition to treatment much easier. A dual diagnosis of BPD and substance abuse can be an uphill battle, but it’s not impossible, and sufferers should not struggle with it alone. Experienced care for BPD symptoms is worth it – remission of BPD symptoms is common after treatment, and there is a low rate of relapse. Once the cycle of addiction and self-medication are conquered, those with BPD can establish new ways to control their lives.
Learn About the Myths & Misunderstandings of Borderline Personality Disorder in the Video Below:
Myths & Misunderstandings of Borderline Personality Disorder from Amanda Wang on Vimeo.
Contact Us For The Treatment Of BPD and Substance Abuse As Co-Occurring Disorders From Maryland Recovery:
Contact Maryland Recovery Today
Reviewed by Christopher Schwartfigure MS, LGPC, CAC-AD








