
Fentanyl is a drug that is used clinically to treat patients who are experiencing high levels of pain, such as cancer patients. While there are many benefits that Fentanyl can bring to the table regarding pain relief it can also be an extremely dangerous substance. It is fairly easy for the body to become dependent on this drug; worse, as Fentanyl is very powerful, it is extremely easy to overdose.
Here, you can find information, on what Fentanyl is, Fentanyl overdose rates, and other facts about Fentanyl.
What Is Fentanyl?
Fentanyl is an opioid-type drug that was created to provide pain relief. As early as 3400 BCE, resinous substances derived from the natural opium poppy plant were found to help relieve pain. In the centuries since, societies have refined this substance, eventually creating a class of pharmaceutical drugs known as opiates. These drugs include well-known pharmaceutical compounds like morphine and codeine.
Synthetic opiate analogues, known as opioids, were created in the mid 20th century. Like natural opiates, these drugs interact with and chemically bind to the body’s opioid receptors to block the pain response. If misused, opioids can trigger the release of pleasurable chemicals known as endorphins, which can produce euphoria and lead to addiction. Synthetic opioids like fentanyl, methadone, and buprenorphine have pharmaceutical purposes while heroin, another synthetic, does not.
Is Fentanyl Dangerous?

Fentanyl is an extremely potent drug, up to 50 times more powerful than heroin and 100 times more powerful than morphine. It only takes a small amount to have a great effect, which is what makes it so dangerous. Amounts as small as two milligrams have the ability to cause an overdose that may lead to death.
Worse, fentanyl cannot be seen, tasted, or smelled. That makes it easy to give to someone without their knowledge, at least until it is too late. Another dangerous aspect of fentanyl is its relatively low cost on the street for a potent effect; people who illegally manufacture and sell street drugs may disguise it as another drug that they can sell for a higher price, which poses an alarming risk to those who consume it unknowingly.
Forms
When produced by a licensed, reputable drug manufacturer and prescribed by a physician, fentanyl may be found in four main forms, including injections, skin patches, nasal sprays, and lozenges similar to cough drops.
When sold illegally, fentanyl can be found as a powder, pressed in the form of small candies or pills, as a liquid in eye droppers, or even as nasal sprays. In 2022, it became popular for fentanyl tablets to be disguised as brightly colored tablets and sold to minors. Many parents and guardians had a difficult time telling the difference between the tablets and candy because they looked so similar.
Some common street names for fentanyl include Apache, China Girl, China Town, Dance Fever, Great Bear, He-Man, Jack Pot, King Ivory, Murder 8, and Tango & Cash.
Mixing Fentanyl and Other Drugs
As mentioned, fentanyl works by binding itself to opioid receptors in the brain that control pain and emotions. By doing so, it can alter the body’s response to pain to a level that many other pain relievers cannot. Unfortunately, it can also create a euphoric high.
In illegal circumstances, fentanyl may be mixed with heroin, cocaine, methamphetamine, and MDMA, also known as Ecstasy. These drugs can work together to create an extended, multifaceted, addictive high that the human body can learn to crave. Because fentanyl is dangerous in even the smallest of dosages, it is easy to overdose quickly. When fentanyl is added to these drugs in unknown amounts, it can cause opioid addiction and overdose even if the individual is unaware they’ve consumed an opioid.
Fentanyl-Related Deaths
More than 150 people die daily from overdoses related to synthetic opioids such as fentanyl. This makes opioids the leading cause of overdose-related deaths in the United States. Unfortunately, it is nearly impossible to tell whether another drug or other substance is laced with fentanyl. Fentanyl strips are one of the only ways to know for sure if a substance contains the drug, but many people are either unwilling or unable to take such precautions.
Since 2015, deaths related to overdoses in general have been rising in the United States, as have fentanyl-related overdoses. In the state of Maryland specifically, fentanyl is now the leading cause of overdose-related deaths. A sharp rise in fentanyl use that began in 2013 has not slowed down since, touching even the younger generations with promises of experiential highs – and severe overdose risks.
Fentanyl Overdose Statistics

Statistics can be helpful in understanding the reality of an issue.
Below are some statistics that may help you build your understanding of the fentanyl misuse issue as a whole.
- In the state of Maryland, the number of deaths related to Fentanyl has spiked dramatically since 2015. The number of deaths related to Fentanyl in 2015 was 340, whereas in 2020, it was 2,342.
- As of 2023, the city of Baltimore had begun reporting a rate of 174 drug overdoses per 100,000 people, with the majority of deaths being caused by fentanyl.
- In the year 2024, the age range that is most affected by opioid overdoses in Maryland is the 35- to 44-year-old age range, with the 25- to 34-year-old age range following closely behind.
- The city of Annapolis reports the highest number of overdoses compared to other cities in Maryland.
While statistics change month by month and year by year, trends are sometimes difficult to break once they are developed over the course of a long period of time. Awareness of a problem such as the rising opioid epidemic is the first step in helping each individual in the United States toward recovery.
Laws Concerning Fentanyl
National laws regarding fentanyl make it legal to manufacture and distribute the drug, including if done by a physician. At the state level, Maryland has its own laws concerning the drug. If you are found guilty of having manufactured, sold, or distributed Fentanyl, you could receive up to 20 years of incarceration and a $20,000 fine. If you are caught transporting just four grams of the drug across state lines, you could be incarcerated for up to 25 years and face a $50,000 fine. This is due, once again, to the potency of the drug.
Fentanyl and Substance Use Disorder
Substance use disorder, the clinical term for addiction, is a condition in which an individual abuses a substance uncontrollably even though it is harmful to their body. Over time, the body and brain have become accustomed to functioning in the presence of drug-related chemicals and the drug may even have stood in for natural chemicals to influence bodily functions. Someone with this disorder cannot function in everyday life without using the substance, even if they are aware of the detrimental effects it is having on their livelihood and health.
Individuals with a substance use disorder like opioid use disorder experience changes in their brains, which alter their ability to make decisions and exercise good judgment. This makes it extremely difficult for them to stop taking opioids. The longer a substance is used, the more serious the damage that is being done and the greater effect it has on the body and the brain.
How Fentanyl Addiction is Treated
Stopping fentanyl use can be difficult to near impossible to achieve on your own. If you stop taking the drug abruptly, your body can respond negatively, causing undesirable symptoms known as withdrawal. It can be very difficult to withdraw from fentanyl or any other synthetic opioid. It is often recommended that those experiencing withdrawals from this drug do so under the oversight of medical professionals.
Some of the symptoms of withdrawal include:
- Irritability
- Muscle and bone pain
- Inability to rest and sleep
- Uncontrollable movement of the legs
- Nausea
- Vomiting
- Diarrhea
- Fever
- Opioid cravings
While these symptoms seem daunting, they can be overcome with the proper treatment and medical care. Medication-assisted treatment (MAT) involves carefully prescribed, FDA-approved medications to stand in for the opioids and ease withdrawal symptoms. The worst of the symptoms typically lasts for about a week, while the lesser symptoms, such as insomnia and anxiety, may last for months. Navigating this process while under medical supervision can not only prevent misuse of MAT drugs but also ensure you deal safely with withdrawal symptoms and build the skills necessary to start a new life free from opioids.
Signs of Overdose
With fentanyl being a rising problem in the United States, as well as in Maryland, it is important to be aware of the warning signs of fentanyl overdose. If an overdose is treated in time, someone’s life could be saved.
Some of the common symptoms of overdose include:
- Constricted pupils
- Passing out or losing consciousness
- Discoloration of the lips and nails,
as well as other parts of the skin - Slowed breathing or stopped breathing altogether
- Choking or gurgling sounds
- Clammy skin that is cold to the touch
- Lack of strength
- Limp body
If you notice these symptoms in someone you believe may be experiencing an overdose of fentanyl, you should follow these steps.
- Immediately call 911.
- If you or someone near you has access to Naloxone (Narcan), administer it as quickly as possible. This will counteract the Fentanyl.
- Help the person onto their side so as to keep them from choking.
- Keep the person awake and encourage them to breathe.
Reversing the Effects of Fentanyl
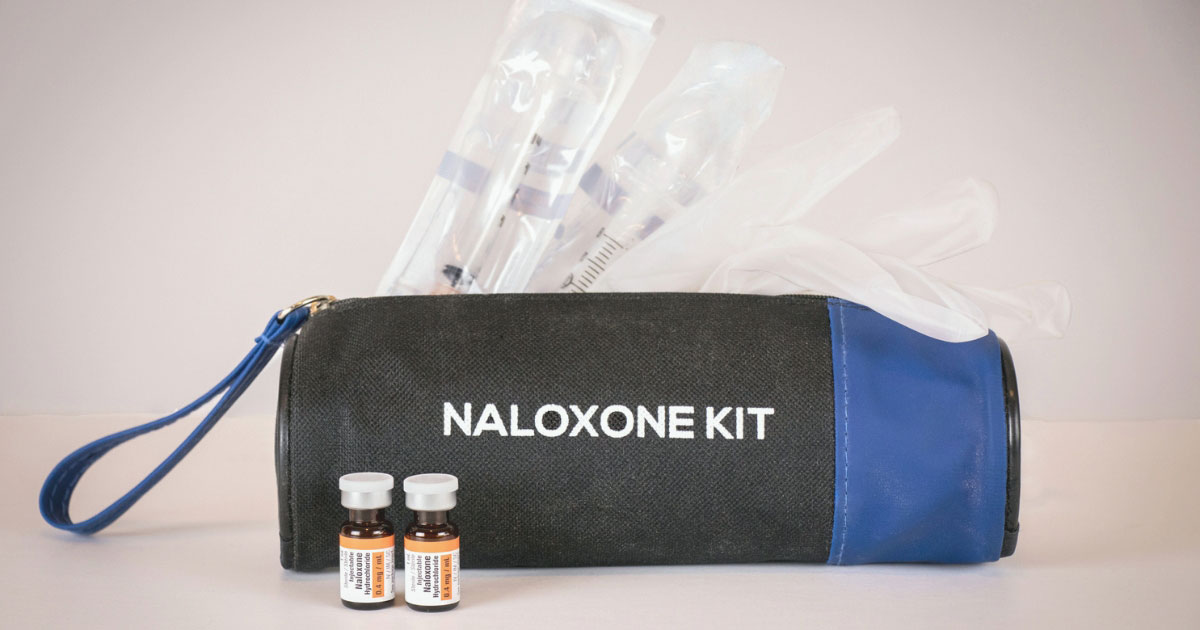
While the effects of fentanyl overdose can be extremely damaging, there is a medication that can reverse those effects if it is administered in time. Naloxone, brand name Narcan, is a medication that is available without a prescription in the United States. You can purchase it in the form of a nasal spray or as an injection. Narcan is completely safe to use and can be administered without a doctor’s approval.
Narcan works by blocking the effects that fentanyl has on the brain while simultaneously restoring the body’s ability to breathe. It does so by causing the opioid molecules to detach from receptors in the brain, but it does not necessarily last forever. The effects of Narcan can wear off in 30 minutes to an hour, meaning that even when Narcan is administered, it is still essential to seek treatment after an overdose.
Fentanyl and Overdose FAQs
At times, fentanyl can seem like a mysterious phenomenon. Unfortunately, its dangers are all too real. Here are some answers to the most common fentanyl questions.
Maryland Recovery: Finding Hope for Fentanyl Addiction

Maryland Recovery is an outpatient drug and alcohol rehabilitation center that offers a personalized approach in order to help each person on their road to recovery, whether from fentanyl or any other substance. While this is not an easy road to travel, it can be done with the proper education, treatment, and a supportive community by your side. Contact us today to learn more about how we can help.
Sources:
- Centers for Disease Control and Prevention. (n.d.). What is fentanyl? https://www.cdc.gov/opioids/basics/fentanyl.html
- Anne Arundel County Department of Health. (n.d.). Naloxone frequently asked questions. https://www.aahealth.org/behavioral-health/recovery-support-services/opioid-addiction/naloxone-frequently-asked-questions
- Johns Hopkins Medicine. (n.d.). Opioids. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/opioids
- Bouby, L., & Salavert, A. (n.d.). Opium poppy in Europe: Exploring its origin and dispersal during the Neolithic. Antiquity. https://www.cambridge.org/core/journals/antiquity/article/opium-poppy-in-europe-exploring-its-origin-and-dispersal-during-the-neolithic/2EF55CA05436425F48982EF9C405B849
- Drug Enforcement Administration. (2022, August 30). DEA warns brightly colored fentanyl used to target young Americans. https://www.dea.gov/press-releases/2022/08/30/dea-warns-brightly-colored-fentanyl-used-target-young-americans
- Centers for Disease Control and Prevention. (n.d.). Drug overdose deaths. https://www.cdc.gov/drugoverdose/deaths/index.html
- Maryland Matters. (2023, August 17). State, county officials discuss strategies to battle the ever-changing opioid crisis in Maryland. https://www.marylandmatters.org/2023/08/17/state-county-officials-discuss-strategies-to-battle-the-ever-changing-opioid-crisis-in-maryland
- Maryland Criminal Lawyer. (n.d.). Maryland drug lawyer. https://maryland-criminallawyer.com/maryland-drug-lawyer/
- AdCare. (n.d.). Fentanyl withdrawal. https://adcare.com/opioids/fentanyl/withdrawal/
- American Psychiatric Association. (n.d.). What is a substance use disorder? https://www.psychiatry.org/patients-families/addiction-substance-use-disorders/what-is-a-substance-use-disorder
- MedlinePlus. (n.d.). How naloxone saves lives in opioid overdose. https://medlineplus.gov/medlineplus-videos/how-naloxone-saves-lives-in-opioid-overdose/
- Maryland Department of Health. (n.d.). Overdose data. https://health.maryland.gov/vsa/Pages/overdose.aspx
- WBAL-TV. (n.d.). Opioid epidemic database: Baltimore deaths. https://www.wbaltv.com/article/opioid-epidemic-database-baltimore-deaths/44869671
- Anne Arundel County Department of Health. (n.d.). Opioid-related data. https://www.aahealth.org/behavioral-health/recovery-support-services/opioid-addiction/opioid-related-data

A solution focused therapist with over a decade in the helping services, I am attuned to the broad expanse of holistic recovery. My mission is inspired by the work of Joseph Campbell, Dr. Wayne Dyer, and Fr. Joseph Martin. I am well versed in the specific needs of the recovery community and am trained in EMDR.








