The world has only recently begun to recognize the serious and long-lasting effects that traumatic experiences have on an individual. The effects of trauma and PTSD have long been seen in trauma survivors, but the medical community simply did not know how to address the symptoms of post-traumatic stress disorder (PTSD), or how to give care for those afflicted with its symptoms.
Today, trauma-informed care offers a better standard of care for those suffering from PTSD and trauma, but the general public, PTSD sufferers, and the families of PTSD sufferers still need to be educated on why this additional level care is needed.
What is Trauma Informed Care?

How Trauma-Informed Care Helps PTSD and Addiction
Trauma-informed care is simply an organizational structure, treatment framework, and model for treatment that is specific to the needs of those who have experienced trauma, traumatic experiences, are suffering from PTSD, or are suffering from trauma-related mental, physical and emotional symptoms.
The ultimate goal of trauma-informed care is to provide treatment to an individual for an underlying condition, while:
- Realizing – that trauma has a wide impact on an individual, and can affect individuals in a multitude of ways. Trauma-informed counselor should also REALIZE and understand the potential paths for recovery from the underlying conditions.
- Recognizing – what the symptoms of trauma are; not only in the patient, but in family members, staff, and everyone else involved in the treatment process.
- Responding – to care for the traumatized individual by implementing knowledge about trauma into policies, procedures and practices for the treatment of individuals suffering from trauma.
- Re-Traumatization – of the individual is resisted by ensuring that all staff, practices and processes will not exacerbate existing trauma symptoms.
What are the Six Key Principles of Trauma-Informed Care?
Trauma-informed treatment utilizes 6 key principles that are kept general so that any form of treatment-given can conform the principals and those treatment and care can be safe to use on those with trauma, without exacerbating the existing trauma symptoms.
- Safety
- Trustworthiness and Transparency
- Peer Support
- Collaboration and Mutuality
- Empowerment, Voice and Choice
- Cultural, Historical, and Gender Issues
These six key principles of trauma informed care should be implemented into any caregiving or treatment program that is provided for a trauma survivor and those suffering from PTSD.
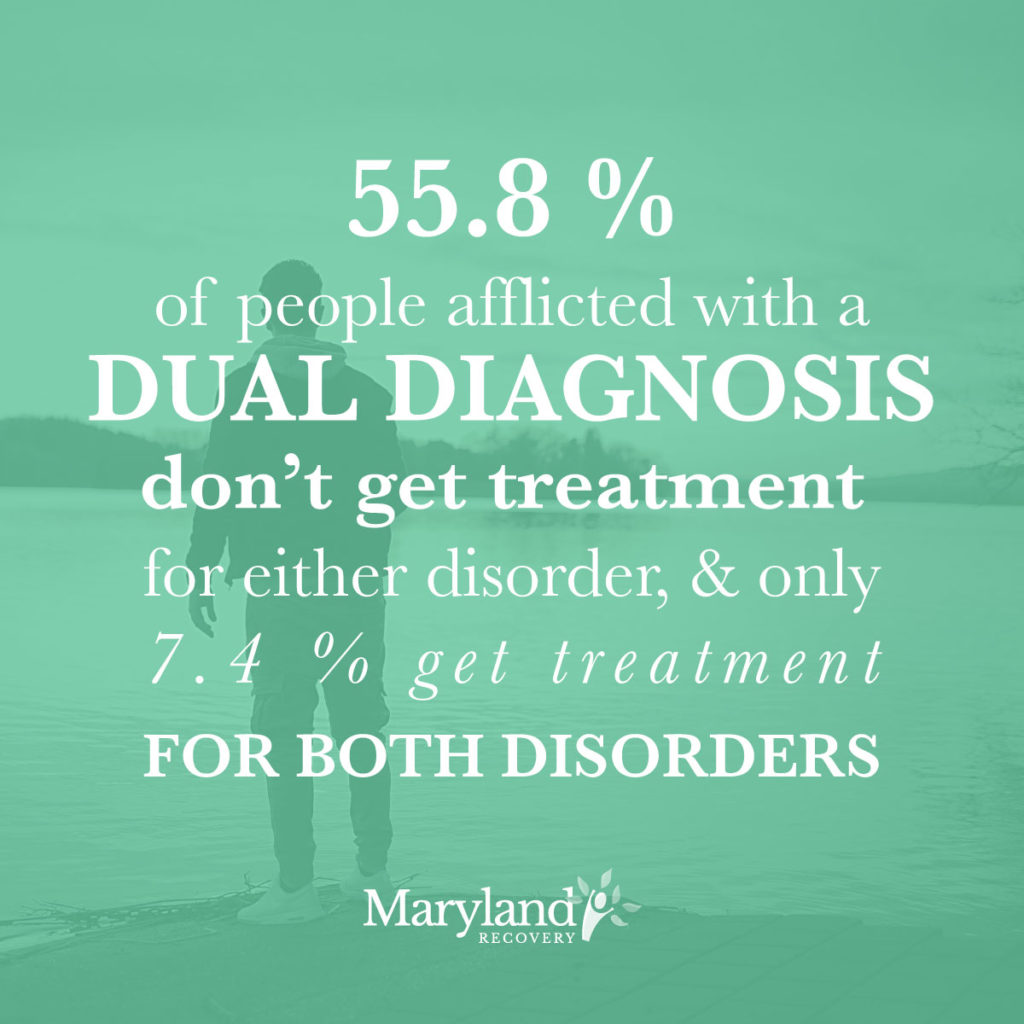
Trauma-Informed Care for Dual Diagnosis Addiction Treatment
Careful steps must be taken in the treatment of any individual that has experienced past traumas, especially when the treatment involves behavioral and mental health treatment. When it comes to substance abuse and addiction treatment in a survivor of trauma or PTSD survivor, the treatment will tackle emotions and issues that surely overlap with the traumatic experience.
In fact, in many cases the trauma itself is directly tied to, or caused the substance abuse and addiction issues. This is why it is so important to make sure that any portion of substance abuse or addiction treatment for PTSD survivors is done with respect to their condition, and utilizes dual diagnosis treatment with trauma-informed care.
Based off the six principles of trauma-informed care, ANY form of treatment given to a trauma patient should utilize trauma informed care. This means that if you are going to provide addiction treatment to a person with PTSD or exposure to trauma, it should be trauma informed treatment.
Why Substance Abuse Treatment with Any Additional Underlying Condition should be treated with Dual Diagnosis Treatment [H2]
Any time a person is struggling with substance abuse or addiction and another underlying condition, the substance abuse/addiction and the other underlying conditions should be treated concurrently (treated at the same time). Why is that? Because holistic treatment should treat the “whole person” not just some symptoms of their conditions.
 Underlying conditions as dual diagnosis can include any of the following:
Underlying conditions as dual diagnosis can include any of the following:
- Substance Abuse/Addiction & Depression
- Substance Abuse/Addiction & Bipolar Disorder
- Substance Abuse/Addiction & Eating Disorders
- Substance Abuse/Addiction & Anxiety Disorders
- Substance Abuse/Addiction & Trauma
- Substance Abuse/Addiction & PTSD
- Substance Abuse/Addiction & Health-Related Illnesses (Cancer, Cirrhosis, Wet Brain, Emphysema, etc.)
Think about it… does it make sense to send your loved one to treat their substance abuse issues in one program, and then send them to another program to treat their eating disorder? No, that would be counterproductive, especially if the eating disorder stemmed from the substance abuse. You would want a medical professional to deal with both interconnected issues at once. That is essentially how dual diagnosis treatment works.
Learn More About Maryland Recovery’s Dual Diagnosis Treatment Program
Treating Substance Abuse and Addiction in PTSD Sufferers
Taking what we know about both trauma-informed care and dual diagnosis treatment one step further, it makes perfect sense to treat a PTSD sufferer (who has a history of substance abuse and a current addiction/chemical dependence) through a trauma-informed dual diagnosis treatment program. Not only will this type of PTSD and addiction treatment program treat all underlying conditions concurrently, but they will do-so according to the principles of trauma-informed care.
This means that your loved one will be in a safe place, with a staff that is informed on trauma-based practices and procedures. Essentially, your loved one will be receiving the proper care, given in a safe environment, by a staff that knows how to give that care pursuant to your loved one’s special needs.
Learn More About Maryland Recovery’s Approach to Trauma &PTSD Treatment
Reviewed by Christopher Schwartfigure MS, LGPC, CAC-AD








