
Triggers and cravings are a completely normal part of recovery. Even though you can expect to experience both as you embark on your healing journey, in the moment, they can seem overwhelming. Instead of allowing triggers and cravings to continue to hound you as you look for sobriety on your own, professional treatment for substance use disorder can provide helpful tools to help you learn how to deal with triggers in recovery.
What Are Triggers?
A trigger is any uncomfortable feeling brought on by a stimulus, like smells, people, thoughts, or circumstances, that causes negative mental, emotional, or even physical symptoms. While people with any mental health condition can experience triggers, in addiction recovery, triggers are especially disturbing because they can bring on memories of painful events as well as previous substance use. As triggers arise, people with substance use disorder often feel a strong desire, also known as a craving, to use substances again.
Triggers can look different for different people; what may trigger one person may not trigger another. But, it is important to note that triggers fall into one of two categories – external triggers and internal triggers. Here are some common examples of both types.
External Triggers
External triggers involve things that occur outside of the person, such as certain situations, people, or places, that remind a person with substance use disorder (SUD) of active substance use and may bring on cravings for the substance of choice.
For example:
- People and Relationships – People who continue to use substances can be a trigger for those who previously did, and even reliving memories of “the good old days” can awaken that familiar urge to use. Similarly, relationships may trigger the urge to return to substance use.
- Places – Certain places that a person may associate with substance use, such as bars, certain restaurants, or clubs, can trigger memories of past substance use.
- Stressful Situations – Stressful circumstances during active substance use often lead individuals to seek unhealthy coping mechanisms like additional substance use. As a result, when someone who is in recovery experiences a stressful situation, it may become triggering.
Internal Triggers
As the phrase suggests, internal triggers involve personal thoughts, feelings, memories, or emotions that create an adverse reaction, which can lead to cravings for the substance of choice. Internal triggers are often tricky to manage, as it can be nearly impossible to stop yourself from feeling negative emotions or remembering unpleasant events.
While everyone has different internal triggers, they commonly arise in these forms:
- Anxiety – Many people in recovery are accustomed to self-medicating anxiety with substances. A resurgence of anxiety can trigger a desire to return to this strategy.
- Depression –Depression is more than just feeling sad; it also involves feelings of hopelessness and lack of motivation. Experiencing these emotions can be a trigger for people with SUD..
- Anger – Feelings of anger can drive a person to substance use, often as an attempt to take control over their life when they feel as though everything else is spiraling out of control.
- Boredom – A lack of positive avenues to release energy and occupy time can lead to unhealthy substance use.
Common Triggers in Recovery
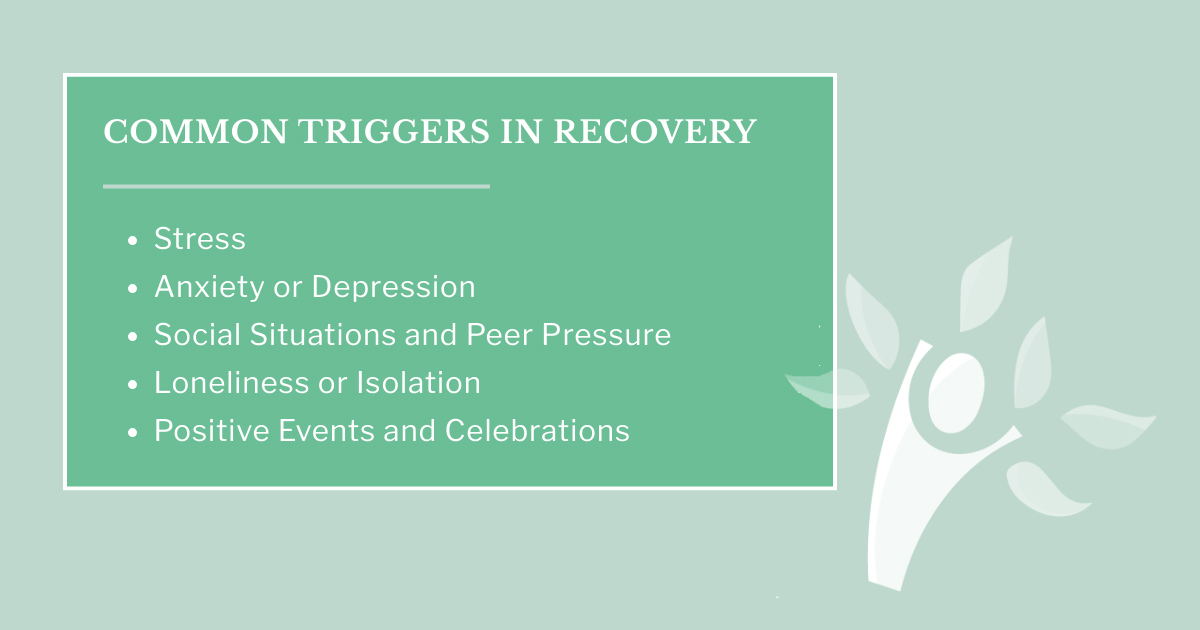
Everyone’s recovery journey looks different, but nearly every person in recovery will experience difficulty at some point. Some of the most commonly experienced triggers of those in recovery include:
Stress
Stress is an expected part of life. When you consider work, raising a family, and financial struggles, it’s clear how many things can become sources of stress. While most people are stressed over these same issues, a person in recovery may have more trouble coping with them, triggering the desire to return to substance use.
Anxiety or Depression
Struggling with anxiety can be crippling, and anxiety is one of the most common triggers during the recovery process. Without undergoing treatment to learn healthy ways of coping with craving, anxiety can lead people to want to use substances again.
Depression is also another common trigger, particularly during the early phase of recovery. People in early recovery are learning how to handle their negative feelings and emotions without the assistance of substances to mask the pain.
Social Situations and Peer Pressure
Going to social gatherings where substances may be available can be a trigger for those in recovery. Sometimes, friends can even put pressure on the recovering person to give in to their triggers. Even reliving memories with friends associated with substance use can trigger a desire to relive that experience.
Loneliness or Isolation
Feeling alone is a trigger experienced by many in their recovery journey. In addition, many people feel uncertain about themselves as they try to create a new sense of normalcy. Conversely, while they may feel alone, the idea of being around others may be exhausting and unappealing.
Creating a support system is essential for remaining in recovery, yet doing so can be both frightening and challenging. Prolonging this critical step can result in further feelings of isolation.
Positive Events and Celebrations
Unfortunately, even positive life events can become triggers for substance use. For example, partaking in substance use may have been a common occurrence at celebrations – some people even view substance use as a celebration in and of itself. Remembering the positive effects of substance use may be another trigger as well.
Why Do Cravings Happen?
Finding recovery from addiction is rarely easy, and remaining in recovery from addiction is even more difficult. The reasons behind these difficulties can often involve cravings. According to a 2016 report from The Office of the Surgeon General, addiction is considered a chronic brain disease (Office of the Surgeon General, 2016).
The connection between the brain and addiction can be explained in three cycles:
- Binge/Intoxication – This first stage describes an individual’s first encounter with substance use, where they have a positive experience due to the temporary feelings of euphoria.
- Withdrawal/Negative Effects – This involves the sudden emotional and physical letdown after the substance is eliminated.
- Preoccupation/Anticipation – The last stage, in which the person searches for substances again (Koob et al, 2004), is a time that is ripe for triggers and cravings.
How Triggers Lead to Cravings
Substances alter the brain in a variety of ways, including elevating dopamine levels beyond normal levels. As the individual continues the substance use, the brain reduces dopamine receptors. This results in the body building up a tolerance to the substance’s effects, so it takes more to experience the same sensations.
Even during recovery, regulating the brain remains difficult, and the very impulsivity and changes in the brain that led to unhealthy coping habits like substance use can remain for quite a while. Experiencing triggers can, in a sense, activate the same old pathways the brain experienced during active substance use and result in cravings for the substance of choice..
Coping Skills to Manage Triggers and Cravings

Both cravings and triggers in addiction recovery are perfectly normal. Rather than worrying about avoiding them completely, it is important to identify triggers and learn healthy ways to manage your triggers and cravings. These are some clinically-supported “best ways” to deal with triggers and cravings:
Use Your CBT/DBT Skills
If you’ve participated in cognitive behavioral therapy (CBT) or dialectical behavioral therapy (DBT), use your new toolkit to help you tackle triggers and cravings. Identify cues by assessing how the emotions you’re currently experiencing reflect the thoughts, circumstances, or even a physical sensation that triggered you. Or, consider the way therapy has helped you begin to identify the negative thoughts that lead to the urge to use substances and reframe them into more helpful ones. As you continue with therapy, take the time to create coping cards, which can remind you of these and other strategies to use to deal with triggers and cravings.
Peer Support Groups
Peer support and/or group therapy are essential resources because they help provide reassurance that you are not alone in your struggles. Better yet, you can learn strategies from people just like you who have put them to good use on their own recovery journeys. Peer support groups can also be an excellent way to develop a support network you can call upon when triggers arise.
12-Step Programs
12-Step programs, such as Alcoholics Anonymous (AA), SMART Recovery, and more, can also be impactful as they provide a structured framework to begin overcoming the unhealthy habits and compulsive decision-making associated with substance use. This resource has existed since the 1930s for good reason – it is a clinically-proven method of managing the ongoing symptoms of a substance use disorder.
Sponsor/Mentor Relationships
Many peer support and nearly all 12-Step programs highlight the benefits of a sponsor/sponsee or mentor/mentee relationship. Sponsors or mentors have the life and recovery experience – and ideally the wisdom – necessary to be a resource you can walk beside along the path to recovery. These experienced individuals can help answer recovery questions, offer support, share experiences, and help keep you accountable and connected with your peer support or 12-Step group.
Sober Support Systems
A solid support system is key to recovery, as it offers encouragement and helps an individual stay on the path when they feel like giving up. Having trusted people to talk to in times of hardship is paramount to success. Support networks can include people like a family physician, close friends, people in a substance use group, counselors or therapists, and family members.
Mindfulness, Meditation, and Breathing Exercises
Meditation and mindfulness are frequently incorporated into holistic addiction treatments that can be very beneficial to those in addiction recovery. These techniques purposefully calm the areas of the brain connected with addictive tendencies and cravings. Likewise, breathing exercises can help you release tension, stress, and trauma, allowing you to experience true healing. In particular, a mindfulness technique known as “urge surfing” can help you focus on the “waves” of your cravings as they become more significant, peak, and then diminish until you’ve successfully let the wave pass over you without succumbing to it.
Healthy Lifestyle Pillars
Returning to a healthy lifestyle is one of the most crucial components of maintaining recovery and dealing with triggers.
These pillars of a healthy lifestyle can help you ensure you give yourself the best chance at mitigating urges:
- Exercise – Establishing a regular exercise routine is an integral part of healthy living and helps your body return to a state where it can benefit your recovery.
- Sleep – Prioritizing sleep by getting about eight hours of restful sleep each night is essential for good health and can help you ensure you aren’t mistaking exhaustion for the urge to use.
- Nutrition – Eating a well-balanced diet is also paramount for a healthy body and can prevent the nutrient cravings that can induce triggers.
- Routine – Developing a consistent, healthy routine can both minimize the downtime that leaves space for cravings and replace the unhealthy habits that previously kept you in active substance use.
Distraction and Delay Plan
In addiction recovery, distraction is a helpful technique to prevent relapse. Distraction and delay plans involve choosing a readily accessible behavior to replace the urge to use substances, and then repeating these practices often to make them a habit.
When you experience a trigger or craving, try the “Four Ds”:
- Delay – Take a few minutes to focus on the craving, delaying your urge to use while you experience the “waves” that often shape cravings.
- Deep Breathing – As the waves continue, practice deep breathing to help them ebb away and dissipate.
- Drink Water – Drink a large glass of water, which not only serves as something healthy to consume rather than alcohol or drugs, but can also address the dehydration that may be causing the craving in the first place.
- Do Something Else – Keep a list of healthy activities you can do most anywhere to help distract you from the craving. These can be as simple as eating a healthy snack or brushing your teeth, or as involved as a nature walk or art project.
Consider Medical Support / MAT
Certain FDA-approved medications can be extremely useful in helping to diminish cravings, especially during early recovery. Medications like naltrexone, buprenorphine, acamprosate, and more can reduce cravings and/or block the chemical receptors necessary to feel the effects of alcohol or opioids. Keep in mind, you must consult a clinician to take part in medication-assisted therapy.
How Treatment Helps
Receiving treatment to aid recovery can make all the difference in your chances of not only finding recovery but maintaining it. Consider these potential components of a personalized treatment plan and how they may help you deal with triggers and navigate them without returning to substance use:
Outpatient Care
Outpatient care offers a structured setting for those who need more support as they enter recovery, without requiring them to stay in the facility at all times. In most cases, outpatient clients are free to attend treatment sessions and return to their home or sober living environment afterward. A significant advantage to outpatient treatment is the flexibility it provides as they slowly adapt to their new chapter in life.
There are more intensive forms of outpatient care available, enabling each individual to access the best fit to address their current needs in their recovery journey:
- Partial Hospitalization (PHP) – This type of program provides individualized substance use disorder (SUD) treatment and frequently coordinates with mental health providers to administer mental health treatment, which means it is ideal for individuals with co-occurring disorders. Typically, this form of outpatient treatment is provided for 5-6 hours per day, seven days per week.
- Intensive Outpatient (IOP) – This type of outpatient treatment program is offered on a more flexible basis than PHP, so individuals must be deemed “clinically ready” for IOP and have limited medical needs. IOP is often ideal for individuals who have already completed residential treatment or detox at another facility, and the best programs offer holistic therapies and relapse prevention strategies.
- MAT – While not a stand-alone outpatient program, medication-assisted treatment (MAT) is frequently used as a component of the above outpatient programs. As mentioned, MAT involves the provision of FDA-approved medications to help reduce cravings and improve the symptoms of withdrawal that so often trigger relapse.
Clinical and Holistic Therapies
Holistic therapy looks different for each individual, for a reason – its components are carefully chosen to meet the individual’s needs. Each treatment aims to care for the whole person, versus addressing symptoms, and enables clients to take control of their health. It also utilizes non-traditional therapeutic and diagnostic strategies while prioritizing the care of the person’s body, mind, and spirit.
Clinically-proven therapies like CBT and DBT can be extremely effective at helping individuals begin to manage the internal thoughts that cause cravings. Other kinds of clinical therapies include group counseling, family counseling, or trauma-informed care. According to research published in Nordic Studies on Alcohol and Drugs, combining holistic therapy with traditional methods, such as a 12-step program, results in positive outcomes for mental health and dependency on substances (Hoyland, et al, 2022).
Long-Term Support
Quality comprehensive outpatient care for those in addiction recovery involves extended care that goes beyond the detox phase. Those who are in the midst of their recovery journey can participate in extended outpatient treatment that feels much like life outside of rehab. Whether sober living accommodations are necessary or a return home is imminent, affordable outpatient care can provide the long-term support needed to maintain recovery.
Triggers and Cravings Don’t Define Your Recovery Journey

Experiencing cravings and triggers is to be expected in the recovery process. Remember: recovery is not about perfection, but rather making progress while implementing healthy coping tools.
For the last 20 years, Maryland Recovery has taken pride in creating addiction recovery programs that pinpoint behavioral and social needs for individuals in recovery. Our aim is to forever change lives with our affordable outpatient addiction treatment solutions. Contact Maryland Recovery’s friendly, compassionate staff and learn more about the options available to you.
*Editor’s Note: This article was originally published January 1, 2015 and has ben updated November 25, 2025.
Sources:
- Koob, G. F., & Volkow, N. D. (2010). Neurocircuitry of addiction. Neuropsychopharmacology, 35(1), 217–238. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805560/
- Addolorato, G., Mirijello, A., Leggio, L., Ferrulli, A., D’Angelo, C., Vonghia, L., … & Gasbarrini, G. (2022). Alcohol use disorder and gut-brain axis: The role of probiotics in healing the microbiota. Frontiers in Psychiatry, 13, 927749. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9549220/
- Lejoyeux, M., & Adès, J. (2005). Mood disorders and suicide: Comorbidity and treatment implications in alcoholism. European Psychiatry, 20(3), 235–240. https://www.sciencedirect.com/science/article/abs/pii/S1566277205000551
- Leshner, A. I. (2016). Addiction is a brain disease, and it matters. In: Volkow, N. D. (Ed.), Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. U.S. Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424849/

A solution focused therapist with over a decade in the helping services, I am attuned to the broad expanse of holistic recovery. My mission is inspired by the work of Joseph Campbell, Dr. Wayne Dyer, and Fr. Joseph Martin. I am well versed in the specific needs of the recovery community and am trained in EMDR.








